Filter
4363
Filtered Results: 4363
Text search:
pregancy
Featured
Recommendations
366
New Publications
1424
Language
Document type
No document type
2884
Guidelines
529
Studies & Reports
462
Manuals
137
Fact sheets
103
Strategic & Response Plan
85
Training Material
68
Infographics
31
Situation Updates
22
Brochures
19
Resource Platforms
11
Videos
7
Online Courses
3
App
2
Countries / Regions
India
261
Kenya
159
Ethiopia
124
Nepal
124
Global
122
South Africa
113
Sierra Leone
102
Uganda
102
Nigeria
95
Zambia
93
Tanzania
91
Malawi
87
Rwanda
83
Liberia
80
Bangladesh
80
Myanmar / Burma
60
Ghana
54
Philippines
52
Latin America and the Carribbean
50
Western and Central Europe
45
Namibia
44
Lesotho
40
Zimbabwe
39
Cambodia
37
Indonesia
36
Africa
33
Senegal
30
Ukraine
29
Congo, Democratic Republic of
28
Haiti
28
Germany
28
Syria
27
Brazil
27
Botswana
25
Russia
24
South–East Asia Region
22
Mozambique
21
Burkina Faso
20
South Sudan
19
Eswatini/ Swaziland
18
Asia
17
Guinea
14
Eastern Europe
14
Cameroon
13
Venezuela
13
Afghanistan
11
Colombia
11
East and Southern Africa
11
Pakistan
10
Benin
10
Yemen
10
Middle East and North Africa
10
Eastern Europe and Central Asia
9
USA
7
West and Central Africa
7
Paraguay
7
Somalia
6
Madagascar
6
Western Pacific Region
6
Mali
5
Lebanon
5
Thailand
5
Argentina
5
Albania
5
North America
5
Côte d’Ivoire / Ivory Coast
4
Sudan
4
Peru
4
Bolivia
4
Southern Africa
4
Laos
4
Georgia
4
Vietnam
4
Turkey
3
Papua New Guinea
3
Burundi
3
Sri Lanka
3
Tajikistan
3
Togo
2
Iraq
2
Jordan
2
Central African Republic
2
North Macedonia
2
Honduras
2
Ecuador
2
Guatemala
2
Bhutan
2
Palestine
2
Moldova
2
Egypt
1
Gambia
1
Ireland
1
Dominican Republic
1
Switzerland
1
El Salvador
1
Greece
1
Libya
1
Angola
1
Mexico
1
Chile
1
Other region
1
Fiji
1
Solomon Islands
1
Armenia
1
Mongolia
1
Congo-Brazzaville
1
Timor Leste/ East Timor
1
Bulgaria
1
Estonia
1
Lithuania
1
Kyrgyzstan
1
Jamaica
1
France
1
United Kingdom
1
Spain
1
Belarus
1
Latvia
1
United Arab Emirates
1
Authors & Publishers
Publication Years
Category
Countries
2054
Women & Child Health
428
Clinical Guidelines
427
Public Health
172
Capacity Building
123
Key Resources
76
Pharmacy & Technologies
18
Toolboxes
HIV
439
COVID-19
250
Mental Health
223
Zika
121
TB
117
Caregiver
116
Refugee
111
Disability
98
Ebola
72
Rapid Response
71
NCDs
70
Conflict
68
Pharmacy
61
NTDs
60
Planetary Health
51
Global Health Education
42
AMR
27
Natural Hazards
21
Health Financing Toolbox
17
Specific Hazards
11
Cholera
9
Polio
7
Social Ethics
6
South Sudan
1
Typhoon
1
Health Financing
1
Recommandations provisoires.
Néanmoins, les femmes enceintes atteintes d’une maladie à virus Ebola évolutive et celles ayant survécu à une telle maladie sans perdre l’enfant à naître sont susceptibles de transmettre le virus pendant l’accouchement et/ou la prise en charge des éventuel...
This article was published on March 4, 2016, at NEJM.org.
DOI: 10.1056/NEJMoa1602412
Please download from the website: http://www.nejm.org/doi/full/10.1056/NEJMoa1602412
Ziel ist es, die Sprachbarriere zwischen Schwangeren arabischer Herkunft und Hebammen, Gynäkologen und Kinderärzten zu überwinden. Der Inhalt wurde aus arabischer und deutscher Fachliteratur entnommen und auf seine Richtigkeit geprueft. Um die Verständlichkeit zu verbessern, wurde bewusst eine e...
Accessed online January 2018
UNAIDS 2016 / Meeting Report
Throughout the gestational period, it is important for obstetric health care facilities to strengthen health counselling, screening, and follow-ups for pregnant women, while incorporating screening, hand hygiene practice, good respiratory etiquette and infection prevention control precautions. These...
Mehr als 160 Artikel und über 300 Kontakte in Südniedersachsen: HEDI verbindet Informationen mit Ansprechpersonen in deiner Nähe. Sicher informiert durch die Schwangerschaft
Mehrsprachig und leicht verständlich. HEDI bietet informative, multimediale Inhalte, die zusammen mit Expert*innen erarbe...
HEDI vernetzt Schwangere und junge Eltern mit Hebammen, Gynäkolog:innen, Kinderärzt:innen und sozialen Anlaufstellen.
Dafür haben wir eine mobil optimierte Web-App entwickelt – kostenlos, werbefrei und mehrsprachig. Die zukünftigen Nutzer:innen waren aktiver Teil dieser Entwicklung. HEDI bea...
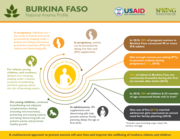
A multisectoral approach to prevent anemia will save lives and improve the wellbeing of mothers, infants, and children
Programmatic update
April 2012
Executive Summary
A finalidade deste documento é apresentar orientações
provisórias para intervenções destinadas a reduzir o risco
de infecção pelo vírus Zika e para tratar potenciais complicações durante a gravidez. Estas orienta ções baseiam-se nas melhores evidências disponíveis da investigação...