Filter
813
Text search:
drug
toxicity
Featured
109
211
Language
Document type
497
155
96
35
16
8
3
2
1
Countries / Regions
62
27
25
17
17
15
14
14
12
11
10
10
9
9
8
8
8
7
6
6
6
6
6
5
5
5
4
4
4
4
4
3
3
3
2
2
2
2
2
2
2
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
Authors & Publishers
Publication Years
Category
283
150
33
32
15
9
9
1
Toolboxes
125
102
61
54
37
34
24
14
13
9
9
8
7
6
5
5
4
2
1
Downloaded from https://aidsinfo.nih.gov/guidelines on 10/19/2019
Recommendations from the National Institutes of Health, Centers for Disease Control and Prevention, the HIV Medicine Association of the Infectious Diseases Society of America and the Pediatric Infectious Diseases Society
(This g
...
Accountability for the global health sector strategies, 2016–2021
WHO/CDS/HIV/19.7
A healthcare worker manual. 2nd edition
The development of this National Manual for the Management of HIV-related Opportunistic Infections and Conditions for use by health care workers at the frontline of our fight against HIV/AIDS is intended to improve their understanding of the causes, preventio
...
Accessed Febr. 6, 2020
Technical Brief
July 2017
Guidelines on post-exposure prophylaxis for HIV and the use of co-trimoxazole prophylaxis for HIV-related infections among adults, adolescents, and children: recommendations for a public health approach : December 2014 supplement to the 2013 Consolidated guidelines on the use of antiretroviral drugs
...
Cancer centres are a major resource in ensuring a comprehensive approach to cancer treatment and its planning. As part of a new roadmap developed by WHO and IAEA to help countries design national cancer control programmes, this publication proposes a framework to develop a cancer centre and/or to st
...
2nd edition. These guidelines include several notable changes from the first edition. For cutaneous leishmaniasis, ketoconazole has been removed from the list of treatment options; the number of Leishmania species for which there is strong evidence for the efficacy of miltefosine has increased from
...
A clear understanding of the knowledge, attitudes and practices (KAP) of a particular community is necessary in order to improve control of human African trypanosomiasis (HAT).New screening and diagnostic tools and strategies were introduced into South Sudan, as part of integrated delivery of primar
...
Despite a historical association with poor tolerability, a comprehensive review on safety of antileishmanial chemotherapies is lacking. We carried out an update of a previous systematic review of all published clinical trials in visceral leishmaniasis (VL) from 1980 to 2019 to document any reported
...
Chagas disease is currently endemic and also predicted to be at increased transmission risk under future climate change scenarios. Similarly, an expansion of areas in the United States at increased risk for Chagas disease transmission is also expected over the next several decades under climate chan
...
Цель этого документа – повысить уровень осознания актуальности приоритетных направлений научных исследований по проблеме ТБ/ВИЧ (то есть по тем направлениям, кот
...
International Journal of Infectious Diseases 32 (2015) 170–178
http://dx.doi.org/10.1016/j.ijid.2014.11.023
1201-9712/ß 2014 The Authors. Published by Elsevier Ltd on behalf of International Society for Infectious Diseases. This is an open access article under the CC BY-NC-ND license (http:
...
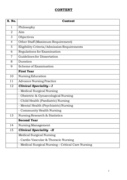
Post Graduate programme is essential to prepare nurses to improve the
quality of nursing education and practice in India. .
Post graduate programme in nursing builds upon and extends competence
acquired at the graduate levels, emphasizes application of relevant theories
into nursing practice, ed
...
TB heroes
Hello, my name is Nurse X
My job is to promote integrated HIV and TB prevention, care, treatment and support. This ensures that we, and my team of health care service providers treat everyone who is living with HIV and TB to have all the antiretroviral therapy (ART) and HIV care services
...
The Millennium Development Goals (MDGs) showed
that global commitment and collective action
could significantly reduce the disease burdens of
three deadly communicable diseases: HIV/AIDS,
tuberculosis (TB) and malaria. The MDGs helped
focus efforts on these three deadly diseases
and leveraged
...