Filter
11276
Filtered Results: 11276
Text search:
Strategie
Featured
Recommendations
896
New Publications
2973
Language
Document type
No document type
6250
Studies & Reports
1938
Guidelines
1321
Strategic & Response Plan
536
Manuals
532
Fact sheets
274
Training Material
170
Situation Updates
106
Resource Platforms
50
Infographics
37
Brochures
28
Online Courses
26
Videos
4
Dashboards/Maps
2
App
2
Countries / Regions
Global
453
India
411
Kenya
319
Ethiopia
232
South Africa
208
Uganda
208
Nepal
201
Nigeria
196
Indonesia
194
Western and Central Europe
191
Sierra Leone
189
Liberia
183
Myanmar / Burma
183
Latin America and the Carribbean
175
Africa
164
Malawi
154
Rwanda
152
Congo, Democratic Republic of
151
Zambia
148
Tanzania
147
Bangladesh
142
Syria
138
Germany
132
Ghana
124
Senegal
112
Ukraine
111
Brazil
93
Venezuela
82
South Sudan
82
Philippines
81
Mozambique
79
Burkina Faso
77
Namibia
77
Eastern Europe
76
Russia
76
Guinea
73
Haiti
72
West and Central Africa
72
Lesotho
67
East and Southern Africa
67
Cambodia
65
Zimbabwe
64
Middle East and North Africa
64
Asia
62
Benin
60
South–East Asia Region
60
Colombia
58
Yemen
53
Paraguay
52
Cameroon
51
Argentina
47
Peru
46
Botswana
46
Central African Republic
43
Lebanon
35
Afghanistan
33
Eastern Europe and Central Asia
33
Pakistan
33
Sudan
28
Chile
26
Bolivia
26
Mali
26
Madagascar
26
Eswatini/ Swaziland
26
Thailand
23
Jordan
21
Somalia
21
Tajikistan
20
Western Pacific Region
20
USA
19
Ecuador
19
El Salvador
17
Côte d’Ivoire / Ivory Coast
17
Vietnam
17
Angola
16
China
15
Niger
15
Iraq
15
Albania
13
Laos
13
Moldova
13
Sri Lanka
13
Guinea-Bissau
12
Burundi
11
North America
11
Turkey
10
Papua New Guinea
10
Georgia
10
Italy
9
Southern Africa
9
Palestine
9
Chad
9
Togo
8
North Macedonia
7
Kyrgyzstan
7
Libya
7
Timor Leste/ East Timor
6
Kazakhstan
6
Iran
6
Hungary
6
Jamaica
6
Portugal
6
Honduras
6
Mexico
5
Gambia
5
Uzbekistan
5
Morocco
5
Armenia
5
Saudi Arabia
5
Turkmenistan
5
Tunisia
5
United Kingdom
5
Spain
5
Egypt
5
Romania
5
Poland
5
Bhutan
5
Guatemala
5
Switzerland
4
Estonia
4
Malaysia
4
Japan
4
Belarus
4
Serbia
3
Canada
3
Singapore
3
Uruguay
3
France
3
Mauritius
3
Bosnia and Herzegovina
3
Fiji
2
Mongolia
2
Qatar
2
Bulgaria
2
Dominican Republic
2
Croatia
2
Lithuania
2
Ireland
2
Gabon
2
Belgium
2
Israel
2
Nicaragua
2
Djibouti
2
Slovakia
2
Greece
2
North Korea
1
Austria
1
Denmark
1
Maldives
1
Norway
1
Algeria
1
Morocco
1
Azerbaijan
1
French Guyana
1
Eritrea
1
Authors & Publishers
Publication Years
Category
Countries
4693
Clinical Guidelines
659
Public Health
594
Women & Child Health
493
Key Resources
461
Capacity Building
207
Pharmacy & Technologies
66
Annual Report MEDBOX
3
Toolboxes
COVID-19
1073
HIV
818
Mental Health
816
TB
614
Planetary Health
455
Disability
440
Conflict
312
AMR
306
Ebola
290
Rapid Response
288
Caregiver
262
NCDs
242
NTDs
241
Refugee
234
Global Health Education
221
Natural Hazards
136
Pharmacy
123
Health Financing Toolbox
100
Zika
73
Polio
68
Cholera
67
Specific Hazards
50
Social Ethics
47
Typhoon
7
Health Financing
3
South Sudan
2
The Democratic Republic of Timor-Leste has the highest TB incidence rate in the South East Asian Region - 498 per 100,000, which is the seventh highest in the world. In Timor-Leste TB is the eighth most common cause of death.
The salient observations are as follows:
In 2018, 487 (12.5%) of the...
Diabetes Burdens: 10.5% adults around the world are currently loving with diabetes.
Evidence shows that oral pre-exposure prophylaxis (PrEP) reduces the risk of contracting HIV during sexual intercourse by more than 90% when taken daily. It is for this reason the National HIV Prevention Strategy 2015-2020 (2018 Revision) emphasises the role of preexposure prophylaxis (PrEP) in ...
On August 13, 2024, the Africa CDC declared the mpox outbreak a Public Health Emergency of Continental Security (PHECS). The following day, the WHO declared it a Public Health Emergency of International Concern (PHEIC). A coordinated, continent-wide response is essential, co-led by the African Union...
This document defines the framework for Malawi’s National HIV Programs. Considering public health benefits and risks, as well as funding and resource implications, deviations from these guidelines are not supported by the Ministry of Health.
Mpox is an emerging zoonotic disease caused by the mpox virus, a member of the Orthopoxvirus genus closely related to the variola virus that causes smallpox. Mpox was first discovered in 1958 when outbreaks of a pox-like disease occurred in monkeys kept for research. The first human case was recorde...
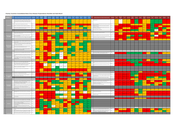
The dashboard is based on assessments made by the International Preparedness Strengthening missions to 14 priority countries against each of the activities outlined in the WHO EVD Checklist at the time of each mission. Updates indicating progress against each of the indicators will be added on an o...
WHO Regional EVD Preparedness Meeting Presentations January 14-16, 2015
The Lancet Global Health: DOI: http://dx.doi.org/10.1016/S2214-109X(16)30098-5
Open Access
Unchecked inequality and failure to protect the rights of poorest women could undermine peace and world’s development goals, new UNFPA report warns:
- Only about half of the world’s women hold paid jobs
- Globally, women earn 77 per cent of what men get
- Three in five women worldwide lack m...
Case study: Cambodia
Lesotho’s predominantly rural population faces significant health challenges within a setting of inadequate human resources for health. It is essential that nurses and nurse-midwives, who together make up the largest health workforce in the country, be adequately prepared to address Lesotho’s He...